*Not all types of atrial fibrillation are suitable for treatment with cardiac ablation or with the FARAPULSE™ Pulsed Field Ablation System. Your doctor will be able to advise you if it could be a suitable treatment for you according to diagnostic and treatment guidelines.
**Study showed 78% of patients free from paroxysmal atrial fibrillation in the first year post cardiac ablation were still free from atrial fibrillation after 4 years.9
REFERENCES:
1.Isabelle C. Van Gelder et al. 2024 ESC Guidelines for the management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS). European Heart Journal (2024) 00, 1–101 https://doi.org/10.1093/eurheartj/ehae176.
2.Reddy VY, Gerstenfeld EP, Natale A, et al. ADVENT: Pulsed Field or Conventional Thermal Ablation for Paroxysmal Atrial Fibrillation New England Journal of Medicine (August, 2023)
3.Ghzally Y, Ahmed I, Gerasimon G. Catheter Ablation. [Updated 2023 Jul 30]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470203/. Accessed July 2024.
4.Sebag FA, Wright M. Cardiac Electrophysiology: Evolution of the technique over the last decade. e-journal of Cardiology Practice 2022 12 Jan;21(15). Available at https://www.escardio.org/Journals/E-Journal-of-Cardiology-Practice/Volume-21/cardiac-electrophysiology-evolution-of-the-technique-over-the-last-decade. Accessed July 2024
5.Yang H, Xiang J, Shen J, et al. Global Research Trends of Cryoablation for Atrial Fibrillation from 2002 to 2022: A Bibliometric Analysis. Anatol J Cardiol. 2023 Dec 1;27(12):688-696. doi: 10.14744/AnatolJCardiol.2023.
6.Cardiac Rhythm News. 29 January 2021. Available at: https://cardiacrhythmnews.com/farapulse-gains-ce-mark-for-its-pulsed-field-ablation-system/. Accessed July 2024.
7.European Society of Cardiology press release marking release of international consensus statement on how to treat AF with ablation. Press release available at: https://www.escardio.org/The-ESC/Press-Office/Press-releases/International-experts-agree-on-standards-for-catheter-ablation-of-atrial-fibrillation. Accessed July 2024.
8.Reddy et al., Pulsed Field Ablation of Paroxysmal Atrial Fibrillation: 1-Year Outcomes of IMPULSE, PEFCAT, and PEFCAT II JACC: Clinical Electrophysiology 7.5 (2021): 614-627.
9.Ngo L, Lee XW, Elwashahy M, et al. Freedom from atrial arrhythmia and other clinical outcomes at 5 years and beyond after catheter ablation of atrial fibrillation: a systematic review and meta-analysis. Eur Heart J Qual Care Clin Outcomes. 2023 Aug 7;9(5):447-458. doi: 10.1093/ehjqcco/qcad037
10.Mont L, Bisbal F, Hernandez-Madrid A, Perez-Castellano N, Vinolas X, Arenal A, et al. Catheter ablation vs. antiarrhythmic drug treatment of persistent atrial fibrillation: a multicentre, randomized, controlled trial (SARA study). Eur Heart J 2014;35:501–7.
https://doi.org/10.1093/eurheartj/eht457
11.Wazni OM, Dandamudi G, Sood N, Hoyt R, Tyler J, Durrani S, et al. Cryoballoon ablation as initial therapy for atrial fibrillation. N Engl J Med 2021;384:316-24. https://www.nejm.org/doi/10.1056/NEJMoa2029554
12.Cosedis Nielsen J, Johannessen A, Raatikainen P, Hindricks G, Walfridsson H, Kongstad O, et al. Radiofrequency ablation as initial therapy in paroxysmal atrial fibrillation. N Engl J Med 2012;367:1587–95. https://doi.org/10.1056/NEJMoa1113566
13.Kuniss M, Pavlovic N, Velagic V, Hermida JS, Healey S, Arena G, et al. Cryoballoon ablation vs. antiarrhythmic drugs: first-line therapy for patients with paroxysmal atrial fibrillation. Europace 2021;23:1033–41. https://doi.org/10.1093/europace/euab029
14.Schmidt B, Bordignon S, Tohoku S, et al. 5S Study: Safe and Simple Single Shot Pulmonary Vein Isolation With Pulsed Field Ablation Using Sedation. Circ Arrhythm Electrophysiol. 2022 Jun;15(6):e010817. doi: 10.1161/CIRCEP.121.010817.
15.Turagam MK, Neuzil P, Schmidt B, et al. Safety and Effectiveness of Pulsed Field Ablation to Treat Atrial Fibrillation: One-Year Outcomes From the MANIFEST-PF Registry. Circulation. 2023;148:35–46. DOI:10.1161/CIRCULATIONAHA.123.064959
16.Ekanem, E., Neuzil, P., Reichlin, T. et al. Safety of pulsed field ablation in more than 17,000 patients with atrial fibrillation in the MANIFEST-17K study. Nat Med (2024). https://doi.org/10.1038/s41591-024-03114-3.
17.Füting A, Neven K, Howel D et al. Patient discomfort following pulsed field ablation for paroxysmal atrial fibrillation – an assessment of chest and groin pain using the Numeric Rating Scale. Clin Res Cardiol (2021). 10.1007/s00392-021-01933-9
CAUTION:
This material is for informational purposes only and not meant for medical diagnosis. This information does not constitute medical or legal advice, and Boston Scientific makes no representation regarding the medical benefits included in this information. Boston Scientific strongly recommends that you consult with your physician on all matters pertaining to your health.
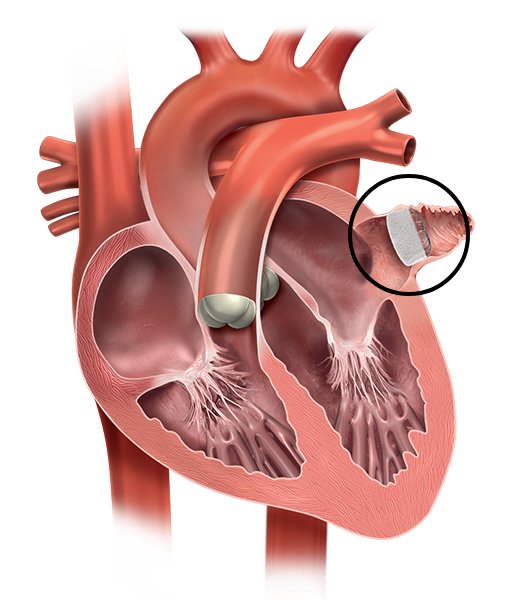
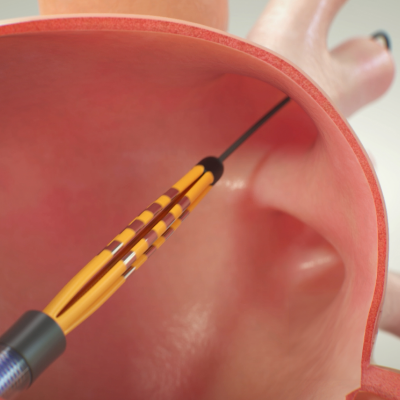
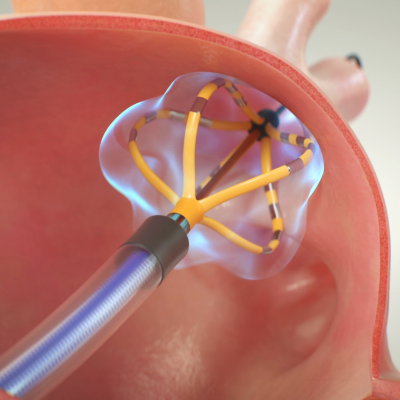
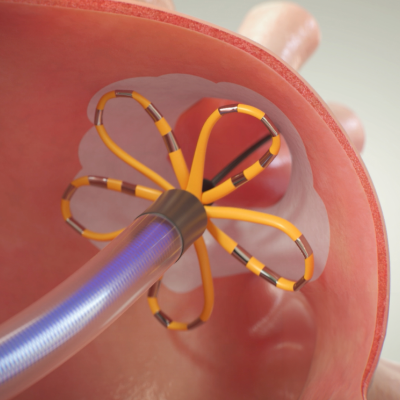
FARAPULSE™ Pulsed Field Ablation System:
The FARAPULSE Pulsed Field Ablation (PFA) System is intended for the isolation of the pulmonary veins in the treatment of paroxysmal atrial fibrillation by rendering targeted cardiac tissue electrically non-conductive to prevent cardiac arrhythmia initiation or maintenance. With all medical procedures there are risks associated with the use of the device. The risks include but are not limited to pain or discomfort, electric shock, hypotension, infection/inflammation, allergic reaction, anesthesia risk, radiation injury/tissue burn, heart failure, renal failure, respiratory distress, arrhythmia, nerve injury (such as phrenic nerve or vagal nerve), gastrointestinal disorders, vessel trauma, cardiac trauma (such as perforation), injury related to adjacent structures (esophageal injury, atrio-esophageal fistula, pulmonary injury), pulmonary vein stenosis, surgical and access complications, muscle spasm, injury due to blood clot or air bubbles in the lungs or other organs, heart attack, TIA, stroke, and/or damage to red blood cells. In rare cases, cardiac arrest or death may occur. Be sure to talk with your doctor so that you thoroughly understand all of the risks and benefits associated with the implantation and use of the device.
All trademarks are the property of their respective owners.